Janet and Susan's Story

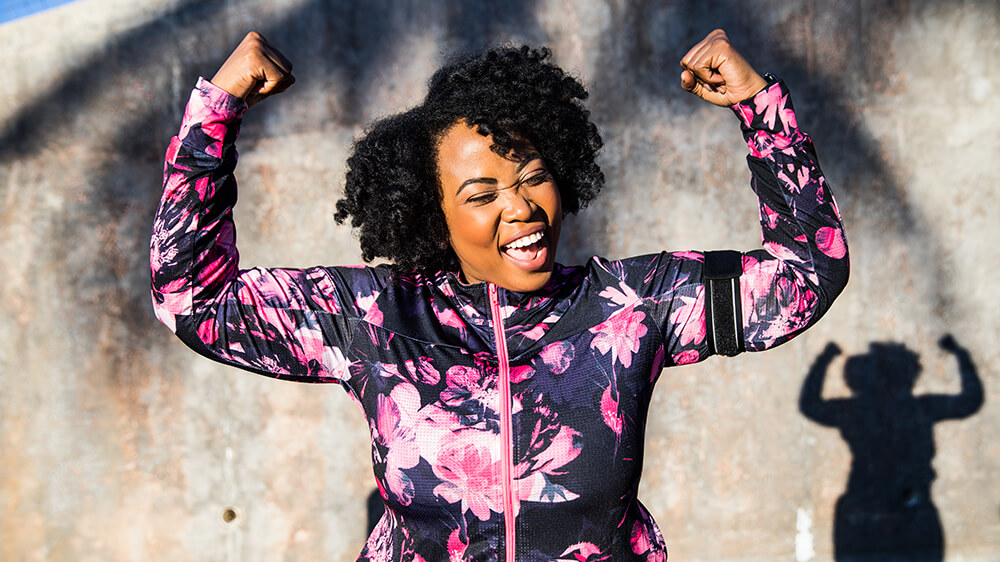
Losing 175 Pounds, Together.
Susan’s Body Mass Index (BMI) — a measure of body size based on height and weight — had climbed to 41, well within the range of Class 3 morbid obesity. “I was horribly embarrassed,” she said. What’s worse, her weight had triggered serious health conditions, including diabetes, high blood pressure, high cholesterol and sleep apnea.
Medical research confirms the two women’s experience: Dieting alone can’t counter obesity. Joseph Greene, MD, co-chair of Holy Cross Germantown Hospital’s bariatric surgery committee, said, “Genetic, physiologic, behavioral and socioeconomic factors — even gender — can create a perfect storm for obesity. It’s not a willpower issue or lifestyle choice. It’s a disease, and we have a treatment for it.”
Now that they have adjusted their fitness and nutrition efforts to align with physical distancing, Janet and Susan continue to lose weight, and credit Holy Cross Health's program with changing their lives. “I feel like I’ve come out of a fog bank into brilliant sunshine,” Susan said. Already, Janet has lost 105 pounds, Susan 70.
Janet and Susan took their first steps in January 2019. They attended a free Holy Cross Health information session and learned about bariatric surgery options, consulted a bariatric surgeon about eligibility — and their journey began.
“Candidates for surgery must have a BMI over 40, or over 35 if other related health problems such as Susan’s are present and most insurance policies will cover it. Surprisingly, one in three people meets this criteria today,” said Dr. Greene.
“Each patient is unique,” said Anuj Prashar, DO, medical director of Bariatric Surgery at Holy Cross Hospital. “Our collaborative, team approach enables us to provide a comprehensive weight loss program that meets the individual needs of each patient to help them achieve long-term weight loss. Healthy, not skinny! That’s the goal.”
Immediately following their screening, Janet and Susan began their preparatory regimen. “It’s a wonderful, holistic process,” said Susan. “We changed our diet, logged our food and water intake, and began pre-operative physician visits.” Janet agreed, “It’s a pretty strict protocol. You meet with a range of specialists — nutritionist, cardiologist and sleep expert.”

“Our lives have changed so much,” Janet said. “I feel so grateful to be on this journey. That Susan and I are on it together is truly a blessing.” -Janet and Susan, Bariatric Surgery Patients
Both women appreciated the program’s attention to psychological drivers of obesity, and began working with its psychotherapist. “There is an emotional component to weight gain,” Janet said. “We realized if we were not committed to dealing with it, we might not succeed.”
Susan and Janet selected one of the two most commonly performed types of bariatric surgery: sleeve gastrectomy, which reduces the size of the stomach to a small pouch. Dr. Greene said selecting the type of bariatric surgery to undergo depends on the individual patient. Their surgeries were performed laparoscopically, which requires only small incisions, speeding recuperation.
Susan’s and Janet’s surgeries were performed a month apart so they could assist each other in post-op recovery — each took approximately two hours. The women scrupulously followed the program’s detailed post-op diet, carefully adding items as instructed. They continue to take advantage of Holy Cross Health support groups, nutritionists and exercise groups, and the support of the bariatric program’s dedicated coordinator.
“Our lives have changed so much,” Janet said. “I see people who are overweight now, and I remember what it was like. I feel so grateful to be on this journey. That Susan and I are on it together is truly a blessing.”